DRSABCD – better known as “Doctors ABCD” – is a common acronym used in first aid training. Although it looks like a bit of a mouthful, DRSABCD is actually an incredibly useful life-saving tool – a procedure that walks you through what to do when you come across someone who might be suffering a Cardiac Arrest.
The letters of DRSABCD stand for Danger, Response, Send for help, Airway, Breathing, CPR and Defibrillation. Each of these is a single step in the first aid process, starting with checking for danger and ending with performing life-saving cardiopulmonary resuscitation (CPR) – and using an automated external defibrillator (AED) if there’s one nearby.
Just knowing the steps doesn’t mean you’re ready to jump straight into a first aid emergency of course. Normally Drs ABCD is taught as part of formal first aid training – it’s an essential part of most first aid courses. So the seven DRSABCD steps are just a way to remember what you’ve learned about what to do in an emergency, and when to do it.
Key Takeaways
- DRSABCD describes the steps to check an unconscious person and start CPR if needed. It’s normally said as “Doctors ABCD”.
- The letters stand for Danger, Response, Send for help, Airway, Breathing, CPR, Defibrillation. Each phrase is a step to complete.
- DRSABCD is most effective when done by someone with first aid & CPR training.
- CPR keeps a cardiac arrest victim alive until medical help can revive them. It won’t restart a person’s heart on its own. Defibrillation is normally needed to revive the person.
- A Defibrillator can revive a person in Cardiac Arrest by momentarily stopping their heart, and allowing it to restart with a more normal rhythm.
- DRSABCD and CPR have saved hundreds of thousands of lives. There are very few negative consequences to doing it, and the benefits far outweigh any risks.
Book Your First Aid Training Today!
HLTAID011 – Provide First Aid | Just $97
HLTAID009 – Provide Cardiopulmonary Resuscitation | Just $50
- Certificate within 24-hours
- Highly Qualified Trainers
- Nationally Recognised Qualifications
Pick A Course From The Selector Below!
So what does DRSABCD stand for?
The seven words or phrases of the DRSABCD process each describe a detailed step in the process of assessing and treating a possible casualty. To provide a brief overview of each term:
- Danger – Check the area for danger (to yourself or others)
- Response – Check the person to see if they conscious and able to respond
- Send for help – Seek medical assistance at once, normally by calling 000
- Airway – Check the person’s airway is clear
- Breathing – Confirm if the person is still breathing
- CPR – Commence cardiopulmonary resuscitation (CPR)
- Defibrillation – Use an AED if one is available
Many of these steps include decisions about what to do next, based on what you learn at that step. For example, you don’t need to commence CPR if someone is still breathing normally, and you shouldn’t approach the person to check for a response if the area is still dangerous.
How is it used?
DRSABCD starts when someone with first aid training enters an area and realises there is a potential casualty – normally someone lying on the ground in an unusual way. It also may start if someone collapses suddenly near the first aider with no clear explanation why.
The steps walk the first aider through the process of finding out what may have happened to the person – starting by checking the area for danger, and then by assessing the person’s condition. It also describes when you should assume the person is suffering cardiac arrest and begin CPR.
A first aider may not perform all the steps of the process – the best-case scenario is that the person is still conscious and in no serious danger. In a way, DRSABCD is the worst-case scenario, explaining what to do with someone who’s unconscious and not breathing – at which point they’re in imminent danger of death.

What does each of the DRSABCD steps mean?
Let’s have a look at each step of the DRSABCD procedure, and what’s involved at each step.
Danger

It reminds first responders that the first thing to do is check for ongoing danger. Although our instinct may be to rush to the aid of someone who’s sick or hurt, it’s important to be cautious. You need to check if there’s an obvious cause for the person’s condition or anything that might cause other injury. Rushing in to help when there’s a venomous snake, exposed electrical wires, or fast-moving traffic nearby could mean you just end up as a casualty yourself.
If you identify danger in the area, you need to remove or control the danger. In some cases, this might involve making changes in the environment – such as switching off electricity or parking your car on the road with hazard lights on. In other cases, it may require moving the casualty. While this isn’t recommended, sometimes it’s unavoidable – performing first aid on someone lying in the middle of a busy expressway is a far bigger risk than moving them.
In some cases, the danger might mean you can’t safely approach. Trying to kill or chase away an angry snake to get to the person they’ve bitten is likely to make the situation far worse. In such cases, you need to keep your distance and call for help.
Once you’ve checked the area and found it to be safe, you can approach the person.
Response

Start with simple questions or requests, speaking in a clear voice. Another common acronym used specifically for this step is COWS – which stands for “Can you hear me?”, “Open your eyes”, “What is your name?”, and “Squeeze my hand, then release it”. Each of these should be spoken to the person in a clear, calm voice to see if they respond. For the last question, you should place your hand in theirs, allowing them to squeeze it if they can.
If the person doesn’t respond to spoken questions, you should try firmly grasping and squeezing their shoulders to see if they respond – making sure that you don’t grasp too hard. When touching the person for any reason, you should make sure you’re not aggravating any existing injuries – or causing any other harm.
If the person doesn’t respond, or shows only a minor response (such as groaning without opening their eyes), you should regard them as unconscious and progress to the next step.
Send for Help
If other people are present, you should ask one of them to call 000 for an ambulance using the closest available phone (normally their mobile, if they have one). This allows you to continue providing aid for the person while they call for help. Once the ambulance has been called, the person can also check the nearby area for an AED unit in case it’s required.
If you are on your own, you should start by calling for help and asking anyone who responds to call an ambulance. If no one is nearby and you have a mobile phone, you can call 000 for an ambulance and place it nearby on speaker phone mode – allowing you to continue providing first aid as you call for help.
Only if there is no alternative should you leave the person to summon help or call for an ambulance – and return as quickly as possible. If the person is suffering Cardiac Arrest then every minute they go without CPR dramatically lowers their chances of survival.
Once you know medical assistance is on the way, you can move on to checking the person’s airway.
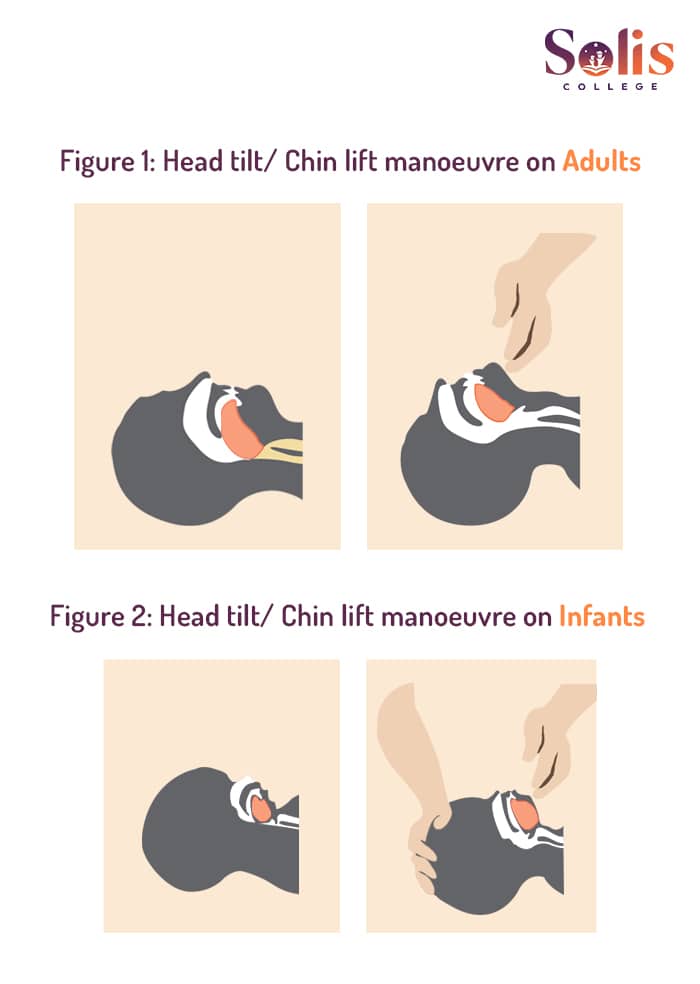
Airway

For adults and children, tilt the head back slightly while lifting the chin (as pictured) to provide the clearest possible path for breathing. For an infant, try to have their head in a neutral position – neither forward, nor backward – as their smaller windpipe can be narrowed if the head is tilted back too far.
Once the airway is correctly aligned, open the person’s mouth and look inside for signs of blockage or fluid (such as water or vomit) in the person’s windpipe. If you find anything, roll the person onto their side (if they’re not in that position already), and allow any foreign material to drain out. Any blockages that do not drain out naturally may be removed with the fingers – sweeping from one side of the mouth to the other.
Be careful when moving the person, particularly if you think they might have a neck injury. But remember that for an unconscious person, ensuring a clear airway takes priority over any other injury.
Once the person’s airway is clear, it is time to assess if the person is currently breathing.
Breathing

Note that movement in the chest may still occur if the person’s airway is blocked – which is why checking the airway first is critical.
Second, move your ear near the person’s mouth and listen for the sound of air escaping from their nose and mouth as they breathe out.
Third, if you can’t hear the air coming in and out of their lungs (perhaps due to nearby noise), see if you can feel the breath coming out.
If the person is breathing normally, this is a good sign. However, if the person is both unconscious and not breathing, they are likely suffering cardiac arrest and you should start CPR.
If someone is breathing abnormally or gasping for air while unconscious or unresponsive, you should still treat them as if they were not breathing and begin resuscitation – regular breathing is essential for life.
CPR

First, ensure the person is lying on their back, and get into a comfortable position beside them – you may be going for a while. Place one hand on the centre of their chest and the other hand on top of it with your fingers interlocked. Then start chest compressions, and rescue breaths – 30 compressions, 2 breaths, and then repeat.
CPR should continue until:
- The person recovers and starts breathing normally
- A medical professional arrives and takes over, or tells you to stop
- You are physically unable to continue
It’s important to note – CPR is a first aid skill, and where possible should be performed by someone with accredited first aid training. Reading a blog (no matter how useful it might be) is no substitute for being properly trained in CPR first aid and practising those skills on a proper training manikin. But we can cover a few fundamentals.
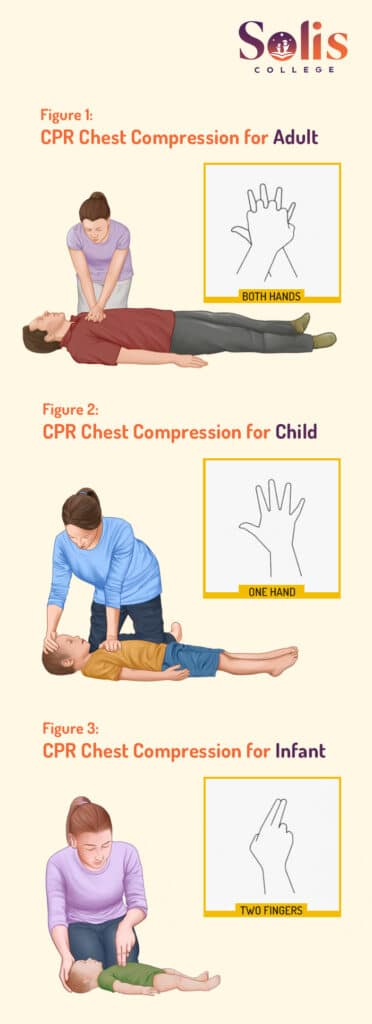
Chest Compressions
When performing chest compressions, push firmly down on the chest so it compresses by around a third – that’s a depth of around 5 cm on an average adult. If unsure, it’s better to push too hard rather than too softly – the danger of CPR not working is far more serious than the danger of injury from someone pushing too hard.
For younger children, often only one hand is needed for compressions, although two hands might be suitable for older children. For an infant, experts recommend using two fingers for compressions as a way to limit how much force you use.
You should be applying chest compressions at around two compressions every second – preferably slightly quicker. One well-known way to keep time is to keep time with the song “Stayin’ Alive” by the BeeGees. Although given that song came out around 50 years ago, younger first aiders might have more luck with songs like “Never Getting Back Together” by Taylor Swift, or “Something Just Like This” by Coldplay and the Chainsmokers. There are lots of options – you just need to choose something you’ll remember.
You should note that performing CPR chest compressions is quite physically demanding, and it is not uncommon for rescuers to grow tired within a few minutes. This can sometimes mean the person’s chest compressions become less effective. For this reason, if there is more than one rescuer present it is a good idea to swap rescuers every two minutes or so – trying to make the changeover as quick and smooth as possible. This allows each rescuer to rest between shifts.
Rescue Breaths
Rescue breaths should be performed from the same position as chest compressions, beside the person. Take a breath, open your mouth as wide as possible, and then place it over the person’s slightly open mouth. Pinch the person’s nose closed, to create a seal (so the air doesn’t simply come out their nose as you blow it in). Breathe out into the person’s mouth (blowing air into their lungs) for around a second – take care not to over-inflate the person’s lungs.
Make sure the person’s chest rises as you blow. If doesn’t, check if the person’s airway has been obstructed somehow. Also check that you are creating enough of a seal on the person’s nose and mouth to prevent air escaping, and you are blowing enough air in.
In some cases it may be easier to close the mouth and blow into the nose, or even to cover both the nose and mouth with your mouth and blow – this is common with infants.
It’s worth knowing that if you’re not able (or willing) to perform rescue breaths, CPR performed with chest compressions only is still effective in many cases. In fact, compression-only CPR is recommended for inexperienced rescuers without CPR training – who may not be confident (or effective) at performing rescue breaths. This is not true in all cases, however – compression-only CPR is not recommended for drowning, drug overdose, or use on children under 9, for example.
What does CPR actually do?
To understand how to use CPR, it’s important to understand what CPR actually does in the body. Many people assume CPR is a way to restart the heart when it’s stopped – pounding on the chest to get the heart pumping again, like someone might bang a faulty machine to make it work. In reality, CPR has almost no chance of “restarting” the heart. It’s actually about keeping the person alive by getting oxygen to their brain.
One of the worst things that can happen to your body is for something to cut off the supply of oxygen-rich blood to the brain. The medical term for someone who has no breathing and no pulse is “clinical death” – unless something extraordinary happens, the person is effectively dead already. In fact, before 20th-century medical procedures such as CPR and Defibrillation, the person would simply be declared dead at that point.
The purpose of CPR is to keep the person alive by supplying oxygen to their brain until medical help arrives. By blowing into the person’s lungs, you force oxygen into their system (yes, the air you breathe out still has a fair bit of oxygen in it). By doing chest compressions, you’re manually pumping the heart, and pushing blood around the body – their veins have valves that keep everything flowing in the right direction. So when their heart and lungs have stopped, you’re getting out of the car and pushing – doing the job of both organs to keep the person alive.
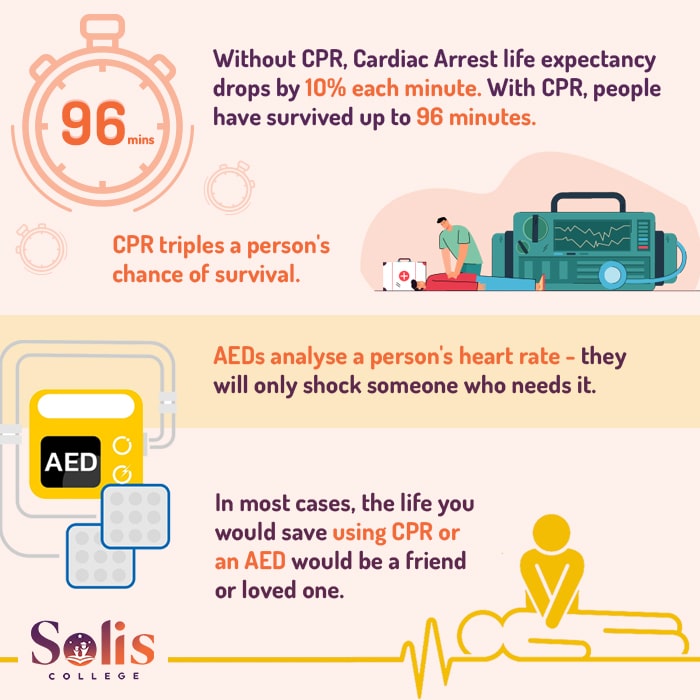
So while you can’t actually revive the person with CPR, you’re keeping them alive for the critical minutes until help arrives. In fact, there are cases of people surviving well over an hour with CPR.
In the case of chest compression-only CPR, this works because generally there’s normally still some oxygen left in the person’s bloodstream, and because pushing down on the person’s chest does push a little bit of air in and out of the lungs. So compression-only CPR is a far better choice than doing nothing. However, it’s far less effective in situations when someone may have been oxygen-starved before you got to them – such as a drowning victim.
Defibrillation

Although ideally a first aider should have been trained with an AED before using one in a medical emergency, most AEDs do come with clear printed instructions. Many modern models also have a voice function, and are designed to clearly talk the user through how to operate them.
They also automatically detect the person’s heart rhythm, detect when a shock is needed, and loudly announce when they’re about to shock and warn users to stand clear. This allows even bystanders with no training to operate one when needed – although obviously they’ll take longer than a trained user, and every second is critical when treating cardiac arrest.
Users should follow the instructions provided by the AED unit to attach the pads to the casualty. Instructions may vary from unit to unit, but some important guidelines are:
- Pads should be placed so that the person’s heart is directly between the two shock pads
- Good skin contact is needed – try to remove excess body hair and wipe away any moisture before applying a pad (but don’t take too long)
- Avoid placing a pad over an implanted medical device – or within 8cm of one (that’s about a hand’s width).
Someone should continue performing CPR while the AED is being fetched and set up, and only stop when the device is ready. Every moment without CPR lessens the person’s survival odds.
It’s worth remembering that unlike in movies and television, real defibrillators do not cause the patient to jerk dramatically when shocked. Nor do they make a loud “thunk” noise – or any sound other than warning noises made by the unit. This idea comes from television and movies, where using a defibrillator is deliberately made more dramatic and visual than in real life. So you don’t need to worry if your AED isn’t working just because the person doesn’t convulse like they do in the movies when shocked.
If the person doesn’t revive after the first shock, continue CPR until the device signals that it’s ready to shock again. Defibrillation doesn’t always work on the first attempt. Sometimes it can take hours.
What does defibrillation actually do?
The common perception of Defibrillation is that you’re using an electrical jolt to jump-start a stopped heart – like someone might jump-start a car engine with jumper leads. In reality, almost the opposite is true. Defibrillation doesn’t start the heart beating – it stops it. In fact, if someone’s heart has stopped entirely, a Defibrillator won’t help them.
In most cases, Cardiac Arrest doesn’t actually mean the person’s heart has stopped entirely. Normally, it means the person is suffering what’s called ventricular fibrillation – their heart is quivering and convulsing erratically, meaning it’s not pumping blood around the body as it would normally.
Defibrillation means giving a very controlled electric shock to stop the heart beating altogether. This then allows the heart to restart by itself a few moments later, returning to a more normal rhythm and starting the flow of blood through the body again – when it works. In a way, it’s less like jump-starting a car and more like turning a machine off and on again in the hopes that it starts correctly and fixes the problem.
If the heart has stopped beating entirely, this is referred to as asystole or cardiac flatline, and at that point, there’s normally not much anyone can do. So yes – all those movies where someone’s heart monitor goes flatline (with that long, drawn-out beep sound) and the hero jumps in to zap them back to life with defibrillator paddles? Yeah, it doesn’t really work like that. That person’s gone.
Book Your First Aid Training Today!
HLTAID011 – Provide First Aid | Just $97
HLTAID009 – Provide Cardiopulmonary Resuscitation | Just $50
- Certificate within 24-hours
- Highly Qualified Trainers
- Nationally Recognised Qualifications
Pick A Course From The Selector Below!
Why is DRSABCD so important?
DRSABCD is an incredibly useful tool that has saved hundreds of thousands of lives over the last half-century. It provides people with a simple way to remember the steps of finding a cardiac arrest victim, assessing the situation, and starting CPR.
In an emergency, it can be easy to panic and forget training or make poor choices. The DRSABCD process gives first aiders a simple, clear process to follow that sums up the knowledge and advice of thousands of medical experts in seven manageable steps.
In Australia, more than 25,000 people suffer a cardiac arrest every year. 90% of those people will not survive. However, it is well known that receiving prompt CPR can triple the chances of survival .
Unfortunately, Australia has one of the worst first aid training rates in the world – in 2017 a study by the Red Cross found only around 5% of Australians were trained in First Aid and CPR. This means that the vast majority of our population is often at a loss for what to do if someone suffers a cardiac arrest near them.
If more Australians had a strong grasp of the steps of DRSABCD and the fundamentals of CPR, it could literally save the lives of hundreds or even thousands of Australians each year.
Are there any risks to following DRSABCD?
When encountering a possible cardiac arrest victim, there are some common concerns people have about starting CPR or using a defibrillator on someone. Will I injure them if I start pushing down on their chest? Could I catch anything doing rescue breaths? Can I get sued for doing CPR if it turns out they don’t need it?
Let’s spend a moment considering these questions.
Could I injure someone by doing CPR or using an AED?
The reality is that it is possible for someone to suffer mild injuries during CPR – the most obvious possibility being bruising or broken ribs from chest compressions. This can make people a little nervous about performing CPR, especially if they’re not sure what might be wrong with the person. However, the recommendation of almost every major medical body is the same – do CPR, and don’t worry about injuries!
Although it is possible to cause minor injuries with CPR, the odds of causing needless injury aren’t high. A 2012 study in Yokohama, Japan examined 910 cases of CPR performed by bystanders. Of those cases, only 26 were found to be unnecessary. Of those, only three suffered any medical complication, including one minor rib fracture. By contrast, the number of lives saved by prompt CPR performed without hesitation was significant. The benefits of prompt CPR far outweighed the risks of accidental injury, even when CPR wasn’t actually needed.
As such, the clear message of the medical community is that on an unconscious person who isn’t breathing, you should run through DRSABCD and perform CPR as soon as possible. Doctors can fix the odd broken rib or bruised chest. They can’t bring someone back from the dead.
As for AEDs, while an advanced hospital Defibrillator could potentially be used incorrectly, AEDs are specifically designed for inexperienced users. They scan the heart rate, and will normally only shock when they’ve detected an irregular heart rhythm in need of Defibrillation. Normally the only way you can be shocked accidentally is by holding onto a person as they’re shocked – which is why AEDs generally give clear warnings to stand clear before they shock anyone.
Can I be sued for doing CPR or using a defibrillator on someone?
No. Although you might have heard horror stories about people in the US being sued for trying to help an injured person, in Australia we have what are called “Good Samaritan laws” to protect people trying to help in an emergency. This means that if you’re providing first aid with the genuine intention of helping people in need, you’re normally protected from legal repercussions.
The laws do vary slightly from state to state. So in New South Wales, for example, a person may not be legally covered if they are the direct cause of someone’s injury. However, it’s worth knowing that as a result of the Good Samaritan laws, no one has ever been successfully sued for providing first aid in Australia.
What about infectious diseases?
This was something people were very worried about during the height of the COVID-19 pandemic. But broadly speaking, while it is possible for an infection to pass from one person to another during CPR rescue breaths, the odds of it happening are very low.
There are various masks and face shields now available for first aiders – including compact CPR face shields that fit on a key chain. So there’s nothing to stop you from making sure you always have a CPR face shield on hand. But the consensus of the medical industry is that the odds of infection are low enough that they’re not strictly needed.
You can use a mask if one is available, but don’t hold off doing rescue breaths because you don’t have one.
Book Your First Aid Training Today!
HLTAID011 – Provide First Aid | Just $97
HLTAID009 – Provide Cardiopulmonary Resuscitation | Just $50
- Certificate within 24-hours
- Highly Qualified Trainers
- Nationally Recognised Qualifications
Pick A Course From The Selector Below!
Why is it called DRSABCD?
If you’ve only just come across the term “DRSABCD”, it might seem like a bit of a mouthful. Although it often helps to know that it’s normally pronounced as “Doctors ABCD” (“Drs ABCD”) rather than spelling out all the letters, you may still wonder why not go with an acronym like “DREAMS” (perhaps standing for “Danger, Response, Emergency call, Airway & breathing, Manual CPR, Shock with AED”).
The answer is that the number of steps has changed over time. In the very early days of CPR, people were only trained to remember “ABC” for airway, breathing, response – given ABC is a very easy group of letters to remember. It was just a simple way to encourage first aiders to verify that a person is able to breathe but not doing so before commencing CPR.
As CPR began to be used more and more by the public, more steps were added to make sure people remembered other important steps of the process – not always in a consistent way. But one of the earliest and most commonly accepted changes was DRABC – or “Dr ABC”, to keep it easy to remember – to remind people to check for danger and see if the person is conscious.
In many medical circles, this was then changed to DRABCD or Dr ABCD – as AEDs became commonly available and usable by the general public, and doctors wanted to encourage people to use them whenever possible. Others used Drs ABC – to make sure people weren’t forgetting to call for medical assistance before starting CPR. Some organisations added other steps that were specific to their needs – such as CABC, which is used by the military to remind soldiers to treat “Catastrophic blood loss” before worrying about airways.
Nowadays, organisations such as the Australian Resuscitation Council (ARC) recommend DRSABCD, or Drs ABCD for first aid and CPR training as it covers the most critical steps, and it’s still relatively easy to remember.
Do I need first aid training to do DRSABCD?
DRSABCD and CPR are both about saving lives. They were developed by medical experts as a way to keep Cardiac Arrest victims alive until help arrives, and they’ve been taught to the general public worldwide as a way to save hundreds of thousands of lives each year (millions of people throughout the world die from Cardiac Arrest each year).
Although many people know about CRP and might even know the basics of DRSABCD, the difference between someone fumbling through an emergency based on half-remembered details from TV, and someone confidently putting their practised first aid skills to use could be seconds or even minutes. And in a CPR emergency, every second is critical, and every minute wasted lowers the person’s survival odds.
There are many benefits to doing a First Aid course and learning CPR and DRSABCD – it looks great on a resume, for example – the most important reason is to have the knowledge and skills to save a life. Although we’d all prefer to never need such skills, you never know when you’ll find yourself in a medical emergency. And remember – if you’re using DRSABCD, the odds are the life you’ll be saving is that of a friend or family member. That’s worth investing a day or two in!
Book Your First Aid Training Today!
HLTAID011 – Provide First Aid | Just $97
HLTAID009 – Provide Cardiopulmonary Resuscitation | Just $50
- Certificate within 24-hours
- Highly Qualified Trainers
- Nationally Recognised Qualifications